A gene known as HbS was the center of a medical and evolutionary detective story that began in the middle 1940s in Africa. Doctors noticed that patients who had sickle cell anemia, a serious hereditary blood disease, were more likely to survive malaria, a disease which kills some 1.2 million people every year. What was puzzling was why sickle cell anemia was so prevalent in some African populations.
How could a "bad" gene -- the mutation that causes the sometimes lethal sickle cell disease -- also be beneficial? On the other hand, if it didn't provide some survival advantage, why had the sickle gene persisted in such a high frequency in the populations that had it?
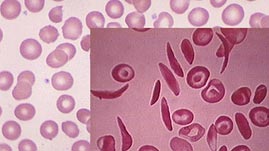
The sickle cell mutation is a like a typographical error in the DNA code of the gene that tells the body how to make a form of hemoglobin (Hb), the oxygen-carrying molecule in our blood. Every person has two copies of the hemoglobin gene. Usually, both genes make a normal hemoglobin protein. When someone inherits two mutant copies of the hemoglobin gene, the abnormal form of the hemoglobin protein causes the red blood cells to lose oxygen and warp into a sickle shape during periods of high activity. These sickled cells become stuck in small blood vessels, causing a "crisis" of pain, fever, swelling, and tissue damage that can lead to death. This is sickle cell anemia.
But it takes two copies of the mutant gene, one from each parent, to give someone the full-blown disease. Many people have just one copy, the other being normal. Those who carry the sickle cell trait do not suffer nearly as severely from the disease.
Researchers found that the sickle cell gene is especially prevalent in areas of Africa hard-hit by malaria. In some regions, as much as 40 percent of the population carries at least one HbS gene.
It turns out that, in these areas, HbS carriers have been naturally selected, because the trait confers some resistance to malaria. Their red blood cells, containing some abnormal hemoglobin, tend to sickle when they are infected by the malaria parasite. Those infected cells flow through the spleen, which culls them out because of their sickle shape -- and the parasite is eliminated along with them.
Scientists believe the sickle cell gene appeared and disappeared in the population several times, but became permanently established after a particularly vicious form of malaria jumped from animals to humans in Asia, the Middle East, and Africa.
In areas where the sickle cell gene is common, the immunity conferred has become a selective advantage. Unfortunately, it is also a disadvantage because the chances of being born with sickle cell anemia are relatively high.
For parents who each carry the sickle cell trait, the chance that their child will also have the trait -- and be immune to malaria -- is 50 percent. There is a 25 percent chance that the child will have neither sickle cell anemia nor the trait which enables immunity to malaria. Finally, the chances that their child will have two copies of the gene, and therefore sickle cell anemia, is also 25 percent. This situation is a stark example of genetic compromise, or an evolutionary "trade-off."
 Loading Standards
Loading Standards Teachers' Domain is proud to be a Pathways portal to the National Science Digital Library.
Teachers' Domain is proud to be a Pathways portal to the National Science Digital Library.