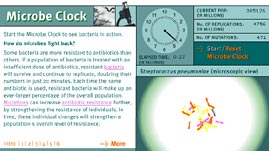
Evolution is often thought of as a process that takes millions of years, but that's not always the case. Single-celled organisms, in particular, ride an evolutionary fast track. Within weeks, a population of bacteria can virtually reinvent itself. In recent decades, this phenomenon has pitted doctors and researchers against mutating bacteria in an anxious battle over antibiotic resistance. Experts now estimate that as many as two dozen types of bacteria have evolved resistance to most, if not all, antibiotics available today. A battle that, thanks to advances in medicine, we have been winning handily for 50 years, appears now to be an even match.
Often it is the chemical structure of individual bacterial cells that enables them to resist the onslaught of antibiotics. If, for example, a patient fails to take a full course of antibiotics, resistant bacteria don't get hit with a dose large enough to kill them. The surviving bacteria enjoy reduced competition, and each time the same antibiotic is used, resistant bacteria make up an ever-larger percentage of the overall population. Mutations can affect antibiotic resistance even more directly, by actually increasing the strength of resistance in individuals. Over time, these individual changes can strengthen a population's overall level of resistance.
Streptococcus pneumoniae, or pneumococcus, is the most common cause of serious infection in the United States. More than 7 million Americans suffer from pneumococcal infections annually; forty thousand of these people die each year. No other bacterium is known to cause more deaths in the United States. Pneumococcus bacteria are spread from person to person through sneezing, coughing, and contact with contaminated surfaces. When a person is first exposed, the bacteria cling to the surface of cells lining the respiratory tract. The most common illnesses caused by
Streptococcus pneumoniae are otitis media (middle ear infection), pneumonia, bacteremia, and meningitis.
Since the early 1940s, antibiotic use has reduced mortality rates among patients with pneumococcal infections by 90 percent. Until recently,
Streptococcus pneumoniae remained extremely susceptible to penicillin and penicillin-like antibiotics. As of 1997, more than half of all pneumococcus bacteria strains were evolving resistance or had become completely resistant to penicillin. The search for alternative antibiotics to treat bacterial illnesses has been only marginally successful.
Strains of at least three other life-threatening bacterial species -- including the species that causes tuberculosis -- have evolved resistance to every available antibiotic, a stockpile of more than 100 drugs. The list of microbes that have developed resistance to at least one antibiotic is growing quickly.

 Loading Standards
Loading Standards Teachers' Domain is proud to be a Pathways portal to the National Science Digital Library.
Teachers' Domain is proud to be a Pathways portal to the National Science Digital Library.